Shorter all-oral regimens for drug-resistant TB cost-effective in India: ICMR study
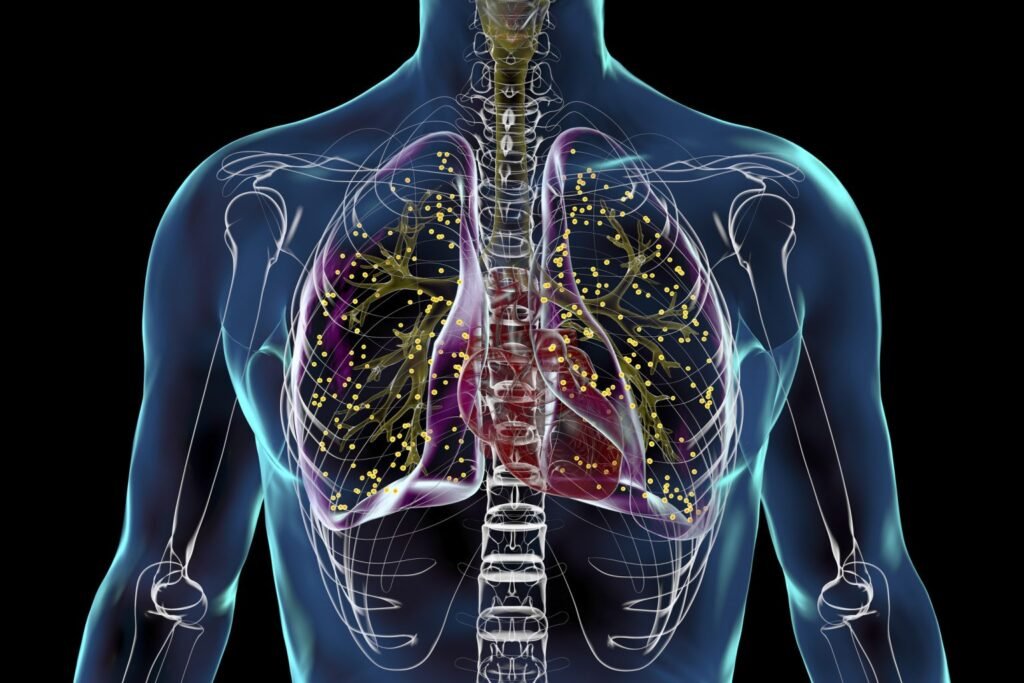
Shorter, six-month all-oral treatment regimens for multidrug-resistant and rifampicin-resistant tuberculosis (MDR/RR-TB) are cost-effective and offer better health outcomes compared to the longer regimens currently in use in India, according to a study conducted by the ICMR–National Institute for Research in Tuberculosis (ICMR-NIRT).
The study, published in the Indian Journal of Medical Research, assessed the cost-effectiveness of bedaquiline-based regimens — BPaL (bedaquiline, pretomanid and linezolid) and BPaLM (bedaquiline, pretomanid, linezolid and moxifloxacin). These were compared with the existing bedaquiline-containing shorter (9–11 months) and longer (18–20 months) treatment regimens implemented under the National TB Elimination Programme (NTEP).
According to the analysis, the BPaL regimen was found to be both more effective and cost-saving. For every additional Quality Adjusted Life Year (QALY) gained, the health system spends Rs 379 less per patient compared to the standard regimen, indicating improved health outcomes at lower cost.
The BPaLM regimen was also deemed highly cost-effective, with an additional expenditure of only Rs 37 per patient per additional QALY gained compared to the standard regimen. Both regimens were associated with lower or comparable overall healthcare costs, including expenditure on medicines, hospital visits and follow-up care.
MDR/RR-TB presents major treatment challenges due to prolonged treatment duration, adverse drug effects and higher costs. The study noted that shorter all-oral regimens can enhance treatment adherence, reduce patient morbidity and enable faster return to normal life, while easing the burden on the health system.
By reducing treatment duration from 9–18 months or longer to six months, the regimens align with national priorities to optimise resource use and accelerate progress towards tuberculosis elimination.
The study found that BPaL-based regimens are likely to be cost-saving or highly cost-effective and may be considered for programmatic adoption under the NTEP to strengthen India’s response to drug-resistant TB.